On 23rd October 2015 the House of Lords debated the Access to Palliative Care Bill, a private member’s bill tabled by crossbench peer Baroness Finlay of Llandaff. The Bill sought to, in her words,
“ensure that wherever a dying person is, whatever the time of day or night, whatever day of the week, they can receive high-standard care… It would do so by ensuring that commissioners commission a level of service for their populations to meet need…My Bill would ensure co-ordination so that help is accessible, efficient and can meet needs.”
The Bishop of Carlisle, Rt Revd James Newcome, who is also lead bishop on healthcare for the Church of England, spoke supportively in the debate.
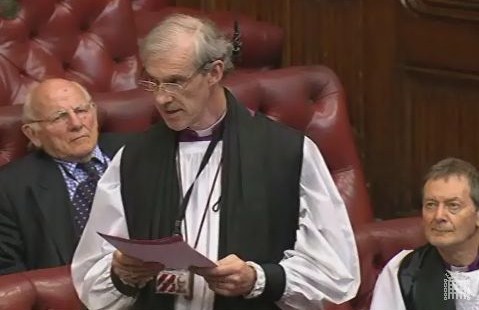 The Lord Bishop of Carlisle: My Lords, I declare an interest as a fairly active patron of Eden Valley Hospice in Cumbria and of Hospice at Home Carlisle and North Lakeland. They work together to provide outstanding end-of-life care for people in the community as well as for those in a hospice bed. Like so many others, I am also most grateful to the noble Baroness, Lady Finlay, for initiating this significant Bill.
The Lord Bishop of Carlisle: My Lords, I declare an interest as a fairly active patron of Eden Valley Hospice in Cumbria and of Hospice at Home Carlisle and North Lakeland. They work together to provide outstanding end-of-life care for people in the community as well as for those in a hospice bed. Like so many others, I am also most grateful to the noble Baroness, Lady Finlay, for initiating this significant Bill.
Reflecting on the now defunct Liverpool care pathway, several medical practitioners of my acquaintance suggested that the real problems lay not in the principle behind it, which was essentially a good one, but in the lack of training given to staff who used it and in the sometimes inadequate way they communicated what was going on, especially to relatives.
Interestingly, training and communication are two of the issues that emerge most clearly from the plethora of recent documents on palliative care, including the ombudsman’s report and those briefings from charities that most of us will have received, however belatedly. They are also two of the issues that are addressed head-on by the Access to Palliative Care Bill, and they have already been mentioned several times today by your Lordships. That is why I want to make training and communication the focus of my brief remarks today.
First, I shall address training. Like end-of-life care itself, as the noble Baroness, Lady Finlay, mentioned in her introduction, and as the noble Lord, Lord Ribeiro, has just explained, the training offered to generalists in this whole area is distinctly patchy. In some trusts it is excellent: indeed, one of the main tasks of a consultant friend of mine who is an end-of-life lead is to educate the whole workforce in her huge hospital. That includes training in electronic care planning and advanced decisions. In other trusts it is not so good and, as a recent article in the Nursing Standard pointed out, a lack of training can be exacerbated by staffing shortages and the stress that results. No wonder the chief executive of Marie Curie says that,
“the government must make training in care of the dying for all health and social care professionals a priority”.
This is addressed in Clause 3 of the Bill.
I should also mention in this context the importance of providing training for prison staff that addresses the particular needs of prisoners and their families. In yesterday’s debate on palliative care, my right reverend friend the Bishop of Rochester indicated that there is some very good practice on this in prison but, as in the wider population, it is inconsistent. With an ageing prison population, it is important to recognise that prison staff and prisoners need some basic understanding of palliative care needs. It would be helpful if this ultimately could be mentioned in the Bill.
I turn to communication. This applies in part to communication across trusts and between members of multidisciplinary teams. Without good communication and close collaboration, people can easily miss out on good end-of-life care plans and specialist support. But it also applies to communication with patients and with their families, which, as the ombudsman’s report makes clear, is sometimes woefully inadequate. The importance of this sort of communication is highlighted by the House of Commons Health Select Committee report, which makes it the second priority of care and indicates that there is occasionally a reluctance on the part of healthcare professionals to talk about end-of-life issues. There is of course an overlap here with training. It is vital that staff should be able to recognise and acknowledge the spiritual dimension of palliative care. In yesterday’s debate I referred to the close link between spirituality and compassion.
Then there is the crucial matter of communication with, and care for, children and adolescents at the end either of their own lives or of the lives of their parents and friends. Palliative care for children has often been neglected in the past, and some major children’s hospitals still have no palliative care team. There is much more that can and no doubt will be said on this very important subject.
I am very glad to give this valuable Bill my warmest support and that of the Church of England. A relatively small initial financial investment, combined with more effective use of existing resources, could make a huge difference to the cost, consistency and overall quality of the care that one day every one of us will need.
(via Parliament.uk)

You must be logged in to post a comment.